Ovarian Cancer Receptor and Growth Factor Genotyping
Triple-Negative Ovarian Cancer (TNEOC):
- Human Epithelial Ovarian Cancer remain one of the leading causes of death in female malignancies[1-4].
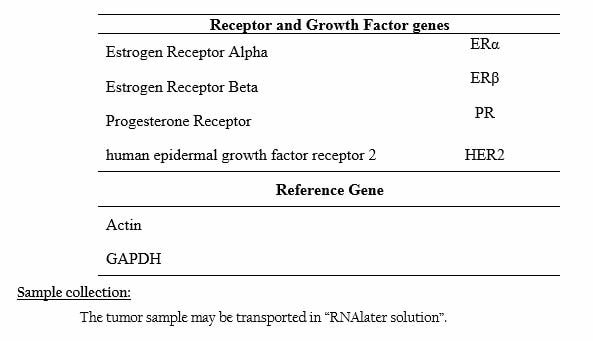
- Estrogen Receptor (ER), Progesterone Receptor (PR) and Human Epithelial Growth Receptor (HER2) are commonly used as prognostic or predictive factors for breast, ovarian and endometrial cancers.
- The absence of the three receptors ER, PR and HER2 results in the triple negative phenotype of cancer.
- The triple negative tumours are known to have defects in DNA repair pathway and are more common in patients with BRCA1 mutation.
- According to a recent study, it was discovered that a subgroup of 15.5% of epithelial ovarian cancers were ‘triple-negative’ in nature proving that the triple negative phenotype was identified in tumours other than breast cancers[5].
- The TNEOC subgroup is correlated with higher histological grade (G3) than non-TNEOC subgroup.
- In breast and ovarian cancers, the triple-negative phenotype was retained as an independent prognostic factor of shorter progression-free survival and overall survival.
- p53, Ki-67 and Epithelial Growth Factor Receptor (EGFR) are known to be markers of aggressive behaviour and poor prognosis in ovarian cancers and furthermore, several studies suggest that TNBC is also positively associated with these prognostic markers [6&7].
- When the expression levels of Ki-67, p53 and EGFR were investigated with TNEOC, it was found that the expression levels of Ki-67 and p53 were higher in TNEOC subgroup than non-TNEOC control[5].
- According to recent studies, ovarian cancer is divided into two subtypes based on gene expression profiles: slow growing subtype I and rapid growing subtype II.
- Subtype I, accounts for 25% of the ovarian cancers and are characterized by low-histological grade and mutations in KRAS, PTEN, and BRAF genes. Likewise, majority of the EOC’s belong to subtype II and are characterized by high level genomic instability and TP53 mutations[8].
- Both type I and type II associated gene mutations were observed in TNEOC tumours.
- Two clinicopathological characteristics, poor prognosis and higher histological grade are common in triple-negative phenotypes.
- Even though the TNBC and TNEOC have some differences, they share most of the clinicopathological and molecular characteristics.
- Loss of PTEN expression and AKT/mTOR signalling pathway overexpression were also frequently observed in human epithelial ovarian cancers [9].
- At present, phase I and II trials are now ongoing with mTOR inhibitors (alone or combined with cytotoxic agents) in ovarian cancer patients [10]
- Recently, a series of phase I-II trials used a PARP pathway inhibitor as therapeutic strategy for BRCA-deficient advanced ovarian cancers, indicating PARP1 inhibitors as candidate treatment options for TNEOC patients [11&12].
- TNEOC should be integrated into the risk factor analysis for epithelial ovarian cancer.
- The accumulating evidences in TNBC research shall provide clues for the search of novel TNEOC biomarkers and targeted therapies.
- Hunn J, Rodriguez GC (2012). Clin Obstet Gynaecol, 55(1):23.
- Jemal A, Bray F, Center MM, et al. (2011). CA Cancer J Clin.;61(2):69–90.
- Barrena Medel NI, Wright JD, Herzog TJ. (2010). J Oncol. 314326.
- Swamy GG and Satyanarayana N. (2010). Nepal Med Coll J, 12(4): 221–223.
- Liu N, Wang X, Sheng X. (2010). J Clin Pathol, 63:240–243.
- Rakha EA, El-Sayed ME, Green AR, et al. (2007). Cancer, 109:25e32.
- Rhee J, Han SW, Oh DY, et al. (2008). BMC Cancer, 8:307.
- Carey L, Rugo H, Marcom S. (2008). J Clin Oncol, 26 (15): 1009.
- Lee YK, Park NH. (2009). Gynecol Oncol, 112:475– 480.
- Trinh XB, van Dam PA, Dirix LY, et al. (2009). Expert Opin Investig Drugs, 18:1885– 1891.
- Fong PC, Yap TA, Boss DS, et al. (2010). J Clin Oncol; 28:2512–2519.
- Audeh MW, Carmichael J, Penson RT, et al. (2010). Lancet, 376:245–251.