Breast Cancer Receptor and Growth Factor Genotyping
Triple-Negative Breast Cancer (TNBC):
- Breast cancer is one of the most common cancer types and the cause of cancer death in women.
- Breast cancer is classified into three subtypes based on the presence/absence of hormone receptors.
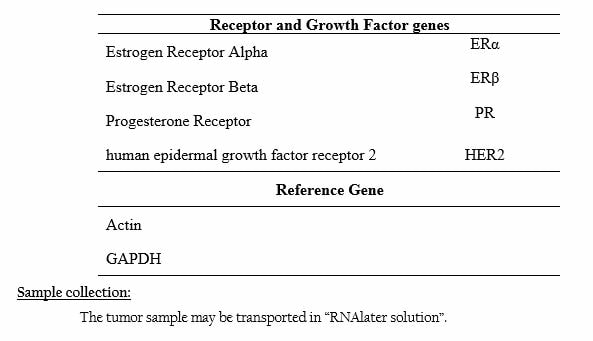
- Which are: Estrogen Receptor (ER), Progesterone Receptor (PR) and Human Epithelial Growth Factor Receptor (HER2).
- Further, breast cancers are classified into five subtypes, based on the receptor expression [1-4]: luminal A and B, normal breast cancer like-, basal like- and claudin-low subtypes [5].
- These breast cancer subtypes are capable of multiplying faster [2-4].
- They are persistent before and after therapy and are consistent between primary tumour and metastasis [5].
- Triple-Negative Breast Cancer is characterized by an absence of the expression of ER, PR and HER2,
- The genes that are normally expressed in basal cells of the normal breast cells are absent in TNBC cells [6&7].
- About 25% of the breast cancer cases are classified as Triple-Negative Breast Cancer.
- TNBC tends to be more aggressive than other breast cancers and are more difficult to treat.
- The extreme risk factor in breast cancer is knowing the hormone receptor status, which will help to know the subtype of breast cancer.
- Nevertheless, knowing the hormone receptor status of the breast cancer will provide a clear view on the cancer status and decide how to treat it.
- Hormone-receptor positive breast cancer cells have either one or both receptors and responds very well to hormone therapy and treatment.
- These cancer cells tend to grow at a slower rate but chances of reoccurrence are greater.
- Hormone-receptor negative breast cancer cells have neither ER or PR, and this makes them difficult to treat with hormone therapy drugs.
- As well as, these cells tend to grow at a faster rate and are more common in women who have not reached menopause.
- TNBC cells do not have any of these hormone receptors attached to them, this makes the TNBC cells more difficult to treat than hormone-positive cells.
- TNBC cells are known for their aggressiveness and out of 100 breast cancer patients 15 patients are affected with TNBC.
- Since hormone therapy doesn’t work on TNBC cells, chemotherapy is still a mainstay of treatment, although patients with triple negative breast cancer have a worst outcome after chemotherapy than patient with other subtypes of breast cancer [8&9]
- There are clinical evidences that shows triple negative indicates the presence of germline mutation of BRCA1 [10&11]
- About 70% of the triple negative breast cancer cases have BRCA1 mutations.
- As BRCA1 mutation carriers age, ER-positive breast cancers become more common [12]
- Apart from BRCA1 mutations, there are five other gene mutations were observed: BARD1, BRCA2, TP53, PALB2 and RAD51D. Several other genes were also identified that moderately increases the risk of TNBC: BRIP1, RAD51C and RAD51D, which were initially considered to be associated with ovarian cancer.
- Perou CM, Sorlie T, Eisen MB, et al (2000). Nature, 406(6797):747–52.
- Sorlie T, Perou CM, Tibshirani R, et al. (2001). Proc Natl Acad Sci USA, 98(19):10869–74.
- Sorlie T, Tibshirani R, Parker J, et al. (2003). Proc Natl Acad Sci USA, 100(14):8418–23.
- Sotiriou C, Neo SY, McShane LM, et al. (2003). Proc Natl Acad Sci USA,100(18):10393–8.
- Weigelt B, Hu Z, He X, et al. (2005). Cancer Res;65(20):9155–8.
- Perou CM, Sørlie T, Eisen MB, et al. (2000). Nature, 406:747-52,
- Rakha EA, Reis-Filho JS, Ellis IO. (2008). J Clin Oncol, 26:2568-81.
- Liedtke C, Mazouni C, Hess KR, et al. (2008). J Clin Oncol, 26: 1275-81.
- Tan DS, Marchío C, Jones RL, et al. (2008). Breast Cancer Res Treat,111:27-44.
- Foulkes WD, Stefansson IM, Chappuis PO, et al. (2003). J Natl Cancer Inst, 95: 1482-5.
- Lakhani SR, Reis-Filho JS, Fulford L, et al. (2005). Clin Cancer Res, 11:5175-80.
- Foulkes WD, Metcalfe K, Sun P, et al. (2004). Clin Cancer Res, 10:2029-34.